Lectio Praecursoria delivered on the occasion of the public examination of my Doctoral dissertation, “Mechanisms of change in psychological treatment of posttraumatic stress symptoms among children and adolescents“, on September 6, 2019, at Tampere University.
According to estimates based on surveys from around 100 countries, a minimum of one billion children and adolescents under the age of 18 are exposed to some form of violence during each year (Hillis et al., 2018). Here they are. Except every one of these symbols represents one million children and adolescents, not one.
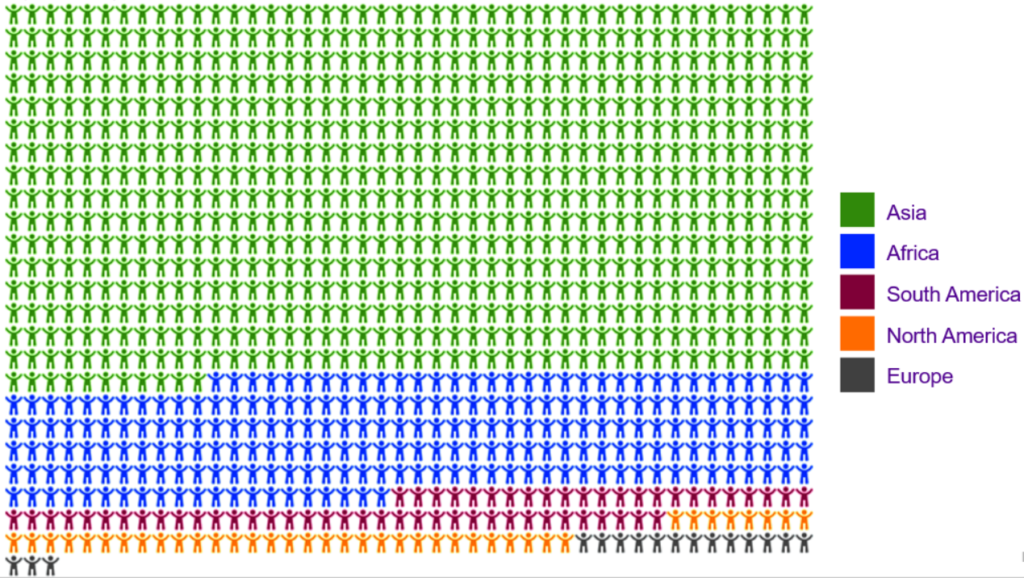
This total estimate includes all forms of violence by all perpetrators, whether adults or other children, from moderate isolated incidents to life-threatening events.
Any exposure to violence can have negative effects on children’s well-being and development.
A notable share of violent events children and adolescents face are also serious enough to be potentially traumatic and cause long-term mental health symptoms. An estimated 30 to 50 percent of people in developed countries may face a potentially traumatic event before they reach the age of 18.
My empirical research focuses specifically on children and adolescents traumatized by repeated exposure to violence in the contexts of war and armed conflict abroad or physical and sexual abuse in Finland.
This year, Save the Children (2019) estimates that 420 million children and adolescents live in areas with on-going war or armed conflict, including 140 million in high-intensity, active conflict zones. In conditions of war, exposure to serious violent events is very common. Children and adolescents may both experience violence themselves and witness violence and atrocities happening to others.
Physical and sexual abuse of children and adolescents also remain pressing problems both globally and in Finland. Around two percent of Finnish adolescent girls and 1.5% of boys report severe physical violence, such as punching, kicking, or battering, from their parents during the last year (Peltonen et al., 2010). This translates to between ten and twenty thousand children and adolescents affected yearly.
Meanwhile, around 5% of Finnish women and 1.5% of men surveyed as adults report having experienced sexual abuse as children (Laaksonen et al., 2011). Although rates of sexual abuse have been declining in Finland in recent decades, this still means between ten and thirty thousand Finnish children or adolescents may have been victims of sexual abuse. Police in Finland register around 1000 cases yearly.
Any exposure to violence is harmful, so we should do all we can to prevent it. Still, children and adolescents often show great resilience and ability to recover. Most children who are exposed to a single violent trauma, research suggests at least three quarters of them, do not develop long-term psychopathology. Assisted by their families, friends, and larger social environment, they are able to process and come to terms with what happened and recover in the weeks and months after the incident.
Unfortunately, in the contexts of physical or sexual abuse or war and conflict, exposure to violence is often repeated. The probability of significant posttraumatic stress symptoms increases steeply with repeated exposure to trauma. Such symptoms include re-experiencing the traumatic event as intrusive memories, flashbacks, or nightmares, hypervigilance, inability to calm down, and conduct problems, as well as avoidance of reminders of the trauma.
In the most difficult conditions where nearly all children have repeatedly witnessed violence, as in the Gaza Strip in Palestine, where some of my research focuses, up to half of all children and adolescents suffer from clinical levels of posttraumatic stress symptoms (Peltonen et al., 2012; Qouta et al., 2012).
Scientific research into posttraumatic symptoms among children and adolescents is a surprisingly recent development. A few decades ago, some researchers still doubted whether children could suffer from such symptoms at all. As late as the 1990s, there was hardly any evidence-based treatment available for children. Our understanding of the impact of trauma and how we may help children and adolescents cope with it has evolved enormously over the last twenty-five years.
By now, clinical trials have demonstrated that psychological treatment of posttraumatic stress symptoms among children and adolescents is possible and can be effective (Dorsey et al., 2017; Gillies et al., 2016). Short-term psychological treatments that specifically focus on the traumatic event or events, and the memories, thoughts and emotions related to them, are able to successfully treat the posttraumatic stress symptoms of most school-age and older children and adolescents. Manualized treatment programs with the most established evidence for effectiveness include Narrative Exposure Therapy, the main focus of my research, Trauma-Focused Cognitive-Behavioral Therapy, and Prolonged Exposure.
We have made much progress in developing treatments. However, several problems do still remain.
Although effective treatments exist, most children and adolescents who suffer from posttraumatic stress symptoms do not receive them. A number of factors contribute to this situation.
First, globally, most violence affecting children and adolescents takes place in low- and middle-income countries, where the availability of resources for mental healthcare is highly limited. This has led to attempts to develop group-based treatments or supportive interventions, as well as interventions that could be implemented by people without formal training in mental health.
Emerging research suggests that psychosocial group interventions may be able to foster and support resilience, provide psychoeducation, or activate peer, parental, and school support. Evidence for their efficacy in directly reducing posttraumatic stress symptoms is, however, mixed, and effects may be quite context-dependent (Brown et al., 2017; Morina et al., 2016, 2017) .
Meanwhile, several studies have found that some trauma-focused individual interventions such as Narrative Exposure Therapy can be successfully implemented by lay counselors, when mental health professionals are not available (Catani et al., 2009; Ertl et al., 2011; Schaal et al., 2009). So far, the use of these interventions has been largely limited to on-going research projects. They are not widely available in low- and middle-income countries.
Even in developed countries, research finds that less than half of children and adolescents with significant posttraumatic stress symptoms receive active treatment (Koenen et al., 2017; Lewis et al., 2019). This is due to both unwillingness or inability to seek treatment, and its limited availability.
Children and adolescents suffering from trauma-related symptoms may understandably be reluctant to engage in treatment where their trauma is discussed in detail. In part, this is due to avoidance of reminders of the trauma, a core part of their symptoms. Beyond that, some children and adolescents, as well as their parents or guardians, believe that negative events in the children’s past are best left alone and not discussed again, even if they do bother the child.
We should of course never force or coerce any child into discussing their trauma. But young trauma survivors with significant symptoms could benefit from additional encouragement and psychoeducation about why discussing their trauma may be helpful and worth the temporary discomfort that may come with it.
Aside from the children and adolescents affected by trauma, the clinicians who meet and assess them are also sometimes wary of offering trauma-focused, and especially exposure-based treatment, even if they have received training in it. Surveys have repeatedly shown that clinicians have concerns about retraumatizing children or otherwise exacerbating their symptoms, if they bring up their trauma (Becker et al., 2004; Deacon et al., 2013). This can sometimes lead to trauma-focused treatment being unnecessarily postponed or never started at all.
Trials of trauma-focused treatment have shown that these concerns, though reasonable, are generally unfounded (Olatunji et al., 2009). Trauma-focused treatment takes training, skill, and courage. But when conducted appropriately, it does not cause harm or pose a risk to trauma-affected children or adolescents, and is instead helpful for many of them.
Even when children and adolescents have access to and begin treatment, not all of them are able to complete it. Typically from around one in ten to one in five drop out. In refining treatment approaches, it would be important to find ways to motivate young patients to stay in treatment and ensure that treatments are not too distressing in the short term.
A significant additional group of young patients, typically around a third, continues to suffer from a substantial level of symptoms even after completing trauma-focused treatment. There is much room to improve the effectiveness of our existing treatments. Treatment-resistant posttraumatic stress disorder is a particular area of concern.
Finally, despite having several treatment programs at our disposal, we still have little understanding of what works best for whom, and under what conditions. Overall, research on treatments for posttraumatic stress symptoms has often found a situation close to what is known in psychotherapy research as the dodo bird’s verdict: “Everybody has won and all must have prizes.”
There is some evidence that trauma-focused treatments are more effective than other types of treatment (Ehlers et al., 2010; Tran & Gregor, 2016). But although different trauma-focused methods differ quite a bit in their emphasis and content, they still appear to demonstrate fairly similar, fairly good effectiveness.
For example, it is still quite unclear whether programs that focus entirely on exposure to the traumatic events and others which mainly concentrate on cognitive restructuring with little or no exposure are really equally effective, and whether one or the other could be more effective for some particular young patients. Similarly, it is unclear whether adding an initial period of stabilization and skills training to trauma-focused treatment is of any particular use.
How can clinical psychological research contribute to improve the current situation and help address these problems? I argue for the importance of two associated lines of research, on which I have also focused on in my Doctoral work.
First, we must increasingly focus on the clinical everyday realities of meeting and treating children and adolescents exposed to trauma, as well as on how treatments are in fact being implemented in usual care. We should study treatments not only in laboratories and clinics attached to universities, but also within existing healthcare systems and structures.
Pragmatic implementation trials are key. With such trials, we may be able to identify barriers to the provision of evidence-based treatment that exist at both clinics and places of treatment in developed countries and in the challenging circumstances of low- and middle-income countries. Further, by studying and developing clinical training, we may be able to assuage concerns clinicians have of using trauma-focused methods, improve their understanding of what may and may not be harmful and what is essential in treating these children and adolescents.
As part of this Doctoral research, I have attempted to contribute to this line of pragmatic research by studying the feasibility of implementing Narrative Exposure Therapy within the Finnish healthcare system, in particular for children and adolescents multiply traumatized by exposure to violence (Peltonen & Kangaslampi, 2019).
Narrative Exposure Therapy is a manualized, short-term individual psychotherapeutic program specifically developed for people who have experienced multiple traumatic experiences during their lifetime (Schauer et al., 2011). We found Narrative Exposure Therapy to be feasible and suitable for use within the Finnish healthcare system, especially so at specialized outpatient units. This form of therapy also reduced posttraumatic stress symptoms at least as effectively and probably somewhat more effectively than forms of treatment previously in use (Peltonen & Kangaslampi, 2019). At the same time, we did uncover some barriers, especially related to the timing of treatment, clinician concerns, and treatment paths that may be addressed in the future to improve access to care.
Second, the focus of clinical trials on psychological treatments needs to move beyond simply showing that treatments are effective into explicitly studying how and why our treatments work, that is, the processes and mechanisms through which treatment can have beneficial effects on the posttraumatic stress symptoms of children and adolescents.
Understanding change in psychological treatment is no simple matter. Treatment features complex interactions between the therapist and the client, influenced by a variety of sources, processes taking place within the client, as well as between the client and his and her environment outside therapy. Because of these complexities, this field of research has sometimes suffered from dissimilar, overlapping, and somewhat confused terminology and research approaches. Sometimes researchers in psychotherapy study the same thing but give it very different names. At other times, they describe the object of their research with the same name, but are in fact studying entirely different processes.
I have found it helpful to ground my research in this framework offered by Brian Doss (2004). He divided what happens in psychological treatment into change processes taking place inside the therapeutic sessions and context, and change mechanisms or mechanisms of change extending outside it.
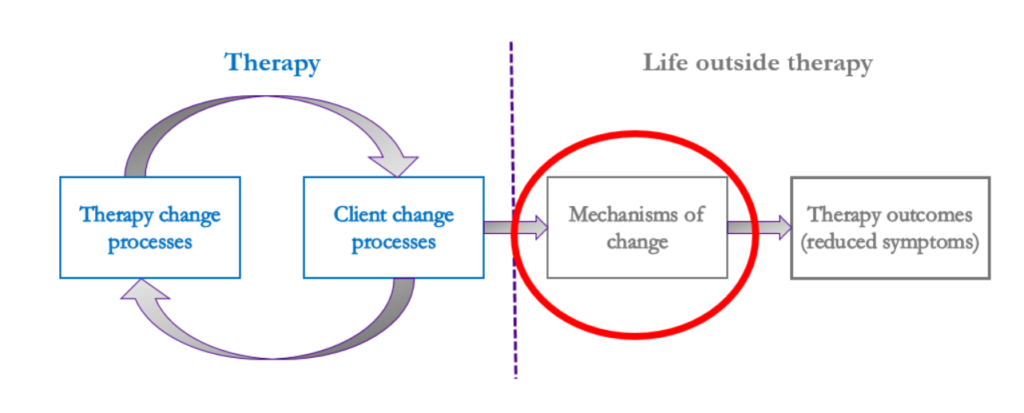
Within therapy, therapist change processes mean everything that the therapist does and says in order to effect change, is, the contents or active ingredients of the therapy. This might mean, for example, the therapist teaching the client new skills and techniques, encouraging the client to talk about their experiences and express their feelings, offering interpretations, or suggesting activities to the client.
By client change processes, Doss (2004) means the responses, behaviors and experiences of the client during the therapy sessions. This might include the client completing activities, using new skills, identifying and working on their thoughts and feelings, or expressing and discussing their experiences and feeling relief.
The main focus of my research, however, has been on those intermediate changes that occur in the client and his or her life outside the immediate therapeutic environment, as a result of what happened inside it. These mechanisms of change refer to changes in the client’s skills, attributes, characteristics, or behavior that have generalized into the client’s life more widely, and which then lead to the desired outcome of the treatment, in this case, reduction in posttraumatic stress symptoms.
Understanding such mechanisms of change could be the key to bringing parsimony to the many different interventions currently in use. Finding out which mechanisms are essential could also assist us in optimizing and better targeting treatments, ensuring the generalizability of treatment effects when we train clinicians and implement treatments in practice, as well as in persuading clinicians to adopt evidence-based treatments.
What might be such mechanisms of change in the case of treating posttraumatic stress symptoms among children and adolescents? We have at our disposal several cognitive-emotional models about why posttraumatic stress symptoms may persist even years after the traumatic event (Brewin et al., 1996, 2010; Ehlers & Clark, 2000; Foa & Kozak, 1986; Foa et al., 2006). These models also make predictions about what should be important pathways to relieving symptoms. In my research, I have mainly focused on two psychological mechanisms.
First, research has demonstrated a close link between posttraumatic stress symptoms and thoughts, beliefs, and appraisals young trauma survivors often have of themselves and the world, which have been negatively and maladaptively affected by their traumatic experiences (Mitchell et al., 2017).
Among children, examples of such trauma-affected thoughts related to the self include “I am a coward.”, “The frightening event has changed me forever.”, “I can’t cope when things get tough.”, “I am no good.” (Meiser-Stedman et al., 2009). Examples of thoughts related to the world and other people could include “Anyone could hurt me.”, “I have to watch out for danger all the time.”, or “I can’t stop bad things from happening to me.” Among others, Anke Ehlers and David Clark (2000) in their cognitive model of posttraumatic stress disorder argue that thoughts and appraisals such as these keep up a sense of continued, current threat among trauma survivors months and years after their traumatic event has passed. This feeling of current threat causes distress and keeps up other symptoms. That is why through changing these thoughts to more adaptive and less negative ones we might also be able to alleviate symptoms.
As part of my Doctoral research, we reviewed all evidence from previous controlled studies on changing such cognitions as a mechanism of change (Kangaslampi & Peltonen, In Press). We found that substantial evidence has indeed accumulated that affecting these thoughts appears to be one key to alleviating posttraumatic stress symptoms by psychological treatment, both among adults as well as children and adolescents. Affecting self-related beliefs may be particularly important. It remains, however, unclear, whether some particular trauma-focused treatments are better at changing them than others.
I further studied the role of these thoughts in the effects of two psychological interventions, Narrative Exposure Therapy as implemented in Finland (Kangaslampi & Peltonen, 2019), and the Teaching Recovery Techniques psychosocial group intervention, as implemented in Gaza, Palestine (Kangaslampi et al., 2016). Together with my colleagues we found that also among multiply traumatized children and adolescents, it appears positive changes in such trauma-affected thoughts during interventions are linked to improvement in symptoms. Inability to affect them may also explain why psychosocial group interventions sometimes appear less successful in relieving posttraumatic stress symptoms.
Our findings further suggest these thoughts and appraisals may be particularly resistant to change among children and adolescents who have repeatedly faced violence. This might be because assessments of the world as dangerous and unpredictable can unfortunately be quite realistic in the uncertain, volatile environments they have grown up in.
As a second possible mechanism of change that especially the dual representation theory of Chris Brewin and colleagues (1996, 2010) places much emphasis on is affecting the nature or quality of the trauma survivor’s memory of their trauma.
Certainly, traumatic memories do appear quite special. They are on one hand easily activated by even remote or peripheral reminders of the trauma, they contain vivid sensory data in all modalities that may be re-experienced in surprising detail, and, when recalled, they have a strong, distressing sense of taking place here and now. On the other hand, traumatic memories may be difficult to describe and sometimes access verbally and consciously. They may be inadequately integrated into autobiographical memory, and they may lack the usual temporal and spatial context of episodic memories.
Dual representation theory (Brewin et al., 1996; 2010) argues that this unusual nature of traumatic memories is what keeps up posttraumatic stress symptoms. Accordingly, by processing the trauma, perhaps we could change these memories into less sensory, more coherent, better integrated and contextualized ones, thereby preventing them from being unintentionally and uncontrollably activated, alleviating symptoms.
In our review we noted that direct evidence of the role of changes in the quality of traumatic memories as a mechanism of change was limited to just one previous study among children and adolescents (Kangaslampi & Peltonen, In Press). In researching the effects of Narrative Exposure Therapy, we did find changes in traumatic memories to associate with symptom reduction (Kangaslampi & Peltonen, 2019). Those children whose memories of their trauma became less sensory, more coherent and better contextualized experienced the most relief in their symptoms. We were not, however, able to provide evidence that this would be a specific mechanism of change involved in Narrative Exposure Therapy.
So, despite emphasis in clinical work, treatment programs, and theory, it remains uncertain whether changing the quality of traumatic memories is really a mechanism through which symptoms could be alleviated, or whether it might be better understood as another possible positive outcome of treatment.
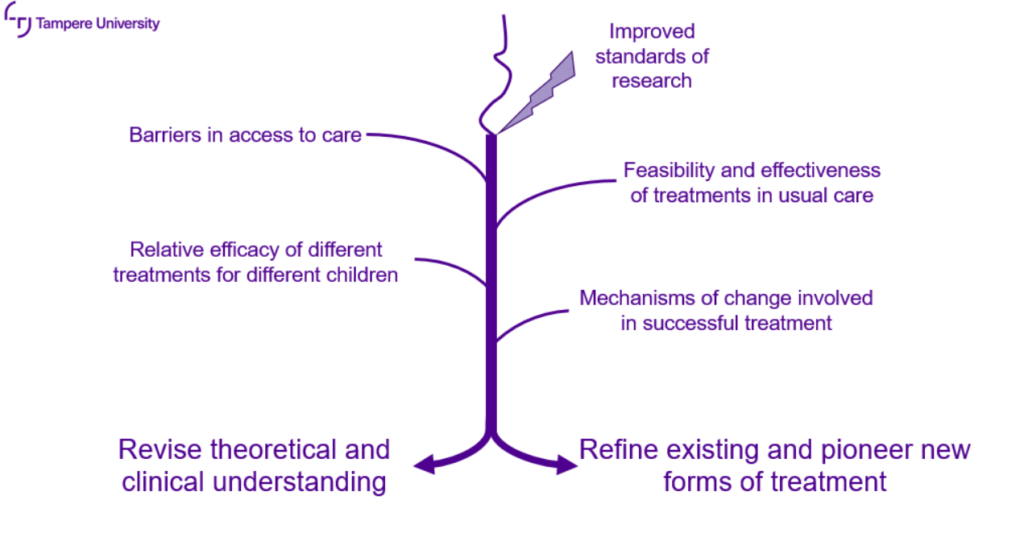
When prevention is not possible, clinicians and researchers owe it to children and adolescents affected by violent traumatic events to offer them the highest level of timely, effective support and care possible. Clinical psychological research can ensure that our understanding of what this highest level of care should entail is based on evidence, not just fallible clinical judgment, good intentions, or high-level theories.
This requires improved standards of research, from careful definition and registration of our hypotheses, to appropriate methods of analysis, and critical consideration of the limitations of our findings. This then requires us to keep collecting evidence on barriers to access to care, on the feasibility of implementing interventions in usual care within current structures, the relative efficacy of different treatments for different groups of children, and on the mechanisms of change involved in successful treatment.
As empirical evidence mounts, this will sometimes also require us to revise our theoretical understanding of what keeps up trauma-related symptoms and how symptoms are best treated, as well as our clinical practices. Finally, this also requires both refining existing forms of treatment and fearless and pioneering work on new, emerging forms of treatment, especially for those children and adolescents who currently do not benefit enough from the treatments at our disposal.
I hope my research has been able to make its own, modest contribution to some of these essential goals.
References
Becker, C. B., Zayfert, C., & Anderson, E. (2004). A survey of psychologists’ attitudes towards and utilization of exposure therapy for PTSD. Behavior Research and Therapy, 42(3), 277–292. https://doi.org/10.1016/S0005-7967(03)00138-4
Brewin, C. R., Dalgleish, T., & Joseph, S. (1996). A dual representation theory of posttraumatic stress disorder. Psychological Reviews, 103(4), 670–686.
Brewin, C. R., Gregory, J. D., Lipton, M., & Burgess, N. (2010). Intrusive images in psychological disorders: Characteristics, neural mechanisms, and treatment implications. Psychological Review, 117(1), 210–232. https://doi.org/10.1037/a0018113
Brown, R., Witt, A., Fegert, J., Keller, F., Rassenhofer, M., & Plener, P. (2017). Psychosocial interventions for children and adolescents after man-made and natural disasters: A meta-analysis and systematic review. Psychological Medicine, 47(11), 1893–1905. https://doi.org/10.1017/S0033291717000496
Catani, C., Kohiladevy, M., Ruf, M., Schauer, E., Elbert, T., & Neuner, F. (2009). Treating children traumatized by war and tsunami: A comparison between exposure therapy and meditation relaxation in North-East Sri Lanka. BMC Psychiatry, 9, 22. https://doi.org/10.1186/1471-244X-9-22
Deacon, B. J., Farrell, C. R., Kemp, J. J., Dixon, L. J., Sy, J. T., … McGrath, P. B. (2013). Assessing therapist reservations about exposure therapy for anxiety disorders: The Therapist Beliefs about Exposure Scale. Journal of Anxiety Disorders, 27, 772–780. https://doi.org/10.1016/j.janxdis.2013.04.006
Dorsey, S., McLaughlin, K., Kerns, S., Harrison, J., Lambert, H., Briggs., E., … Amaya-Jackson, L. (2017). Evidence base update for psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Clinical Child and Adolescent Psychology, 46(3), 303–330. https://doi.org/10.1080/15374416.2016.1220309
Doss, B. D. (2004). Changing the way we study change in psychotherapy. Clinical Psychology: Science and Practice, 11(4), 368–386. https://doi.org/10.1093/clipsy/bph094
Ehlers, A., Bisson, J., Clark, D. M., Creamer, M., Pilling, S., Richards, D., . . . Yule, W. (2010). Do all psychological treatments really work the same in posttraumatic stress disorder? Clinical Psychology Review, 30, 269–276. https://doi.org/10.1016/j.cpr.2009.12.001
Ehlers, A. & Clark, D. M. (2000). A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy, 38, 319–345. https://doi.org/10.1016/S0005-7967(99)00123-0
Ertl, V., Pfeiffer, A., Schauer, E., Elbert, T., & Neuner, F. (2011). Community-implemented trauma therapy for former child soldiers in Northern Uganda: A randomized controlled trial. JAMA, 306(5), 503–512. https://doi.org/10.1001/jama.2011.1060
Foa, E. B., Huppert, J. D., & Cahill, S. P. (2006). Emotional processing theory: An update. In: B. O. Rothbaum (Ed.), Pathological Anxiety: Emotional Processing in Etiology and Treatment. New York, NY: Guilford Press.
Foa, E. B., & Kozak, M. J. (1986). Emotional processing of fear: exposure to corrective information. Psychological Bulletin, 99, 20–35.
Gillies, D., Maiocchi, L., Bhandari, A. P., Taylor, F., Gray, C., & O’Brien, L. (2016). Psychological therapies for children and adolescents exposed to trauma. Cochrane Database Systematic Reviews, 10, CD012371. https://doi.org/10.1002/14651858.CD012371
Hillis, S., Mercy, J., Amobi, A., & Kress, H. (2016). Global prevalence of past-year violence against children: a systematic review and minimum estimates. Pediatrics, 137(3), e20154079.
Kangaslampi, S. & Peltonen, K. (2019). Changes in traumatic memories and posttraumatic cognitions associate with PTSD symptom improvement in treatment of multiply traumatized children and adolescents. Journal of Child and Adolescent Trauma. Advance online publication. https://doi.org/10.1007/s40653-019-00255-3
Kangaslampi, S. & Peltonen, K. (In press). Mechanisms of change in psychological interventions for posttraumatic stress symptoms: A systematic review with recommendations. Current Psychology.
Kangaslampi, S., Punamäki, R.-L., Qouta, S., Diab, M., & Peltonen, K. (2016). Psychosocial group intervention among war‐affected children: An analysis of changes in posttraumatic cognitions. Journal of Traumatic Stress, 29, 546-555. doi: 10.1002/jts.22149
Koenen, K. C., Ratanatharathorn, A., Ng, L., McLaughlin, K. A., Bromet, E. J., Stein, D. J., … Kessler, R. C. (2017). Posttraumatic stress disorder in the World Mental Health Surveys. Psychological Medicine, 47, 2260–2274. https://doi.org/10.1017/S0033291717000708
Laaksonen, T., Sariola, H., Johansson, A., Jern, P., Varjonen, M., von der Pahlen, B., … Santtila, P. (2011). Changes in the prevalence of child sexual abuse, its risk factors, and their associations as a function of age cohort in a Finnish population sample. Child Abuse and Neglect, 35(7), 480–490. https://doi.org/10.1016/j.chiabu.2011.03.004
Lewis, S. J., Arseneault, L., Caspi, A., Fisher, H. L., Matthews, T., Moffit, T. E., … Danese, A. (2019). The epidemiology of trauma and post-traumatic stress disorder in a representative cohort of young people in England and Wales. The Lancet Psychiatry, 6(3), 247–256. https://doi.org/10.1016/S2215-0366(19)30031-8
Meiser-Stedman, R., Smith, P., Bryant, R., Salmon, K., Yule, W., Dalgleish, T., & Nixon, R. (2009). Development and validation of the Child Post-Traumatic Cognitions Inventory (CPTCI). Journal of Child Psychology and Psychiatry, 50, 432–440. https://doi.org/10.1111/j.1469-7610.2008.01995.x
Mitchell, R., Brennan, K., Curran, D., Hanna, D., & Dyer, K. F. W. (2017). A meta-analysis of the association between appraisals of trauma and posttraumatic stress in children and adolescents. Journal of Traumatic Stress, 30(1), 88–93. https://doi.org/10.1002/jts.22157
Morina, N., Koerssen, R., & Pollet, T. V. (2016). Interventions for children and adolescents with posttraumatic stress disorder: A meta-analysis of comparative outcome studies. Clinical Psychology Review, 47, 41–54. https://doi.org/10.1016/j.cpr.2016.05.006
Morina, N., Malek, M., Nickerson, A., & Bryant, R. A. (2017). Psychological interventions for post-traumatic stress disorder and depression in young survivors of mass violence in low- and middle-income countries: meta-analysis. British Journal of Psychiatry, 210(4), 247–254. https://doi.org/10.1192/bjp.bp.115.180265
Olatunji, B. O., Deacon, B. J., & Abramowitz, J. S. (2009). The cruelest cure? Ethical issues in the implementation of exposure-based treatments. Cognitive and Behavioral Practice, 16(2), 172–180. https://doi.org/10.1016/j.cbpra.2008.07.003
Peltonen, K., Ellonen, N., Larsen, H. B., & Helweg-Larsen, K. (2010). Parental violence and adolescent mental health. European Child and Adolescent Psychiatry, 19(11), 813–822. https://doi.org/10.1007/s00787-010-0130-8
Peltonen, K. & Kangaslampi, S. (2019). Treating children and adolescents with multiple traumas: a randomized clinical trial of narrative exposure therapy. European Journal of Psychotraumatology, 10(1), 1558708. doi: 10.1080/20008198.2018.1558708
Peltonen, K., Qouta, S., El Sarraj, E., & Punamäki, R.-L. (2012). Effectiveness of school-based intervention in enhancing mental health and social functioning among war-affected children. Traumatology, 18(4), 37–46. https://doi.org/10.1177/1534765612437380
Qouta, S., Palosaari, E., Diab, M., & Punamäki, R.-L. (2012). Intervention effectiveness among war-affected children: A cluster randomized controlled trial on improving mental health. Journal of Traumatic Stress, 25(3), 288–298. https://doi.org/10.1002/jts.21707
Save the Children. (2019). Stop the war on children. Protecting children in 21st century conflict. Retrieved from https://www.savethechildren.org/content/dam/usa/reports/edcp/stop-the-war-on-children-2019.pdf
Schaal, S., Elbert, T., & Neuner, F. (2009). Narrative exposure therapy versus interpersonal psychotherapy: A pilot randomized controlled trial with Rwandan genocide orphans. Psychotherapy and Psychosomatics, 78, 298–306. https:/doi.org/10.1159/000229768
Schauer, M., Neuner, F., & Elbert, T. (2011). Narrative exposure therapy: A short-term treatment for traumatic stress disorders. (2nd Ed.). Göttingen, Germany: Hogrefe.
Tran, U. S., & Gregor, B. (2016). The relative efficacy of bona fide psychotherapies for posttraumatic stress disorder: a meta-analytical evaluation of randomized controlled trials. BMC Psychiatry, 16, 266. https:/doi.org/10.1186/s12888-016-0979-2